Celiac Disease
Celiac disease is an autoimmune reaction to gluten that remains underdiagnosed. At Vibrant America, we offer a comprehensive panel to help you optimize your treatment outcomes by early detection.
About the disease
Celiac disease is a disorder characterized by intestinal malabsorption of nutrients due to sensitivity to the alcohol-soluble portion of gluten known as gliadin. Wheat, rye, barley, and to a lesser extent, oats contain this protein substance and can induce mucosal damage in the gut causing nonspecific villous atrophy of the small intestine mucosa. Most patients are asymptomatic. This disease has variable clinical manifestations that can lead to severe symptoms such as profound malabsorption, steatorrhea, and wasting. There are associations between celiac disease and Type I diabetes mellitus, thyroid disease and other autoimmune diseases.
Symptoms
Celiac disease in adults
-
Depression or anxiety
-
Iron-deficiency/anemia
-
Fatigue
-
Arthritis
-
Seizures or migraines
-
Bone loss or osteoporosis
-
Irregular menstrual periods
-
Infertility or recurrent miscarriage
-
Dermatitis herpetiformis (itchy skin rash)
-
Mouth Ulcers
-
Tingling or numbness in the hands and feet
-
Bone or joint pain
Celiac disease in children
-
ADHD
-
Failure to thrive
-
Delayed puberty
-
Short stature
-
Irritability
-
Defects of permanent teeth
-
Fatigue
-
Weight loss
-
Pale, foul-smelling or fatty stool
-
Abdominal pain and bloating
-
Chronic diarrhea
-
Vomiting
Genetic Disposition
Celiac disease has a genetic disposition. First relatives of someone diagnosed with the disease have a 1 in 22 chance of having signs of the disease in their lifetime. Uncontrolled celiac disease predisposes patients to gut carcinomas and lymphomas and it is most common in Caucasians of Northern European descent.
Celiac Tests

Celiac disease tests are ordered when someone has signs and symptoms suggesting celiac disease, malnutrition, and/or malabsorption. The symptoms are often nonspecific and variable, making the disease difficult to spot. The symptoms may be mild for some time, going unnoticed, and then progressively worsen or occur sporadically.
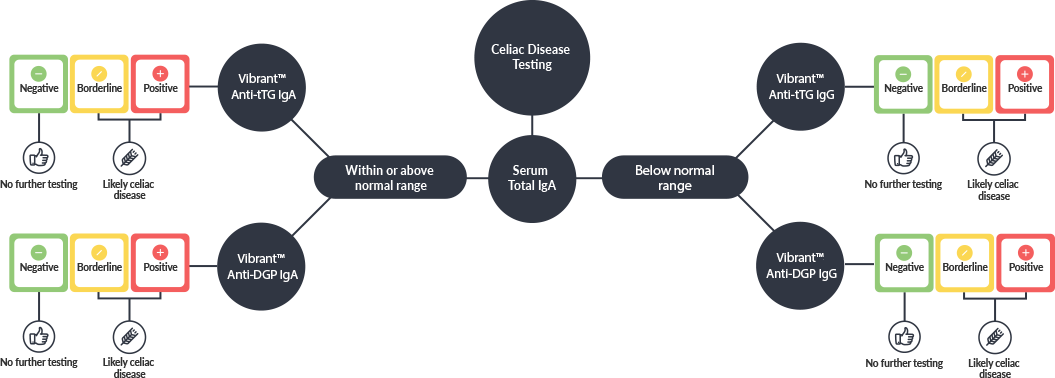
- Vibrant™ Anti-tTg IgA
- Vibrant™ Anti-tTg IgG
- Vibrant™ Anti-dGP IgA
- Vibrant™ Anti-dGP IgG
- Total IgA
Additional Tests
Other tests may be ordered to help determine the severity of the disease and the extent of the complications a person may experience, such as malnutrition, malabsorption, and the involvement of other organs. Tests may include:
HOW DO YOU ORDER VIBRANT’S CELIAC DISEASE TEST?
Vibrant’s celiac disease test is only available to order through your provider. If your physician is not in our network, please contact us.
Results

If the test results indicate absence of antibodies tested for celiac disease, confirm your patient was eating a normal, gluten-containing diet for a least 3 weeks prior to testing. If not, the test results may have been compromised. If the patient was eating normally, there is a chance he/she has non-celiac gluten sensitivity.
Celiac Disease Test Interpretation
This test has been developed and its performance characteristics determined by the CLIA-certified laboratory performing the test. This test has not been cleared or approved by the U.S. Food and Drug Administration (FDA). Although FDA does not currently clear or approve laboratory-developed tests in the U.S., certification of the laboratory is required under CLIA to ensure the quality and validity of the tests.
1. Leffler, D.A. & Schuppan, D. (2010). Update on serologic testing in celiac disease. Am J Gastroenterol. 105 (12):2520-4.
2. Volta U, Fabbri A, Parisi C, et al. Old and new serological tests for celiac disease screening. Expert Rev Gastroenterol Hepatol. 2010;4(1):31-35.
3. Leffler, D.A. (2011). Celiac disease diagnosis and management: A 46-year-old woman with anemia. JAMA, 306(14), 1582-1592.
4. Prince, H.E. (2006). Evaluation of the INOVA diagnostics enzyme-linked immunosorbent assay kits for measuring serum immunoglobulin G (IgG) and IgA to deamidated gliadin peptides. Clin Vaccine Immunol, 13, 594-151.
5. Kumar, V., Jarzabek-Chorzelska, M., Sulej, J., Karnewska, K., Farrell, T., & Jablonska, S. (2002). How Celiac Disease and Immunoglobulin A Deficiency: How Effective Are the Serological Methods of Diagnosis? Clinical and Vaccine Immunology, 9(6), 1295-1300.


